The very real risks of opioid dependence in Australia

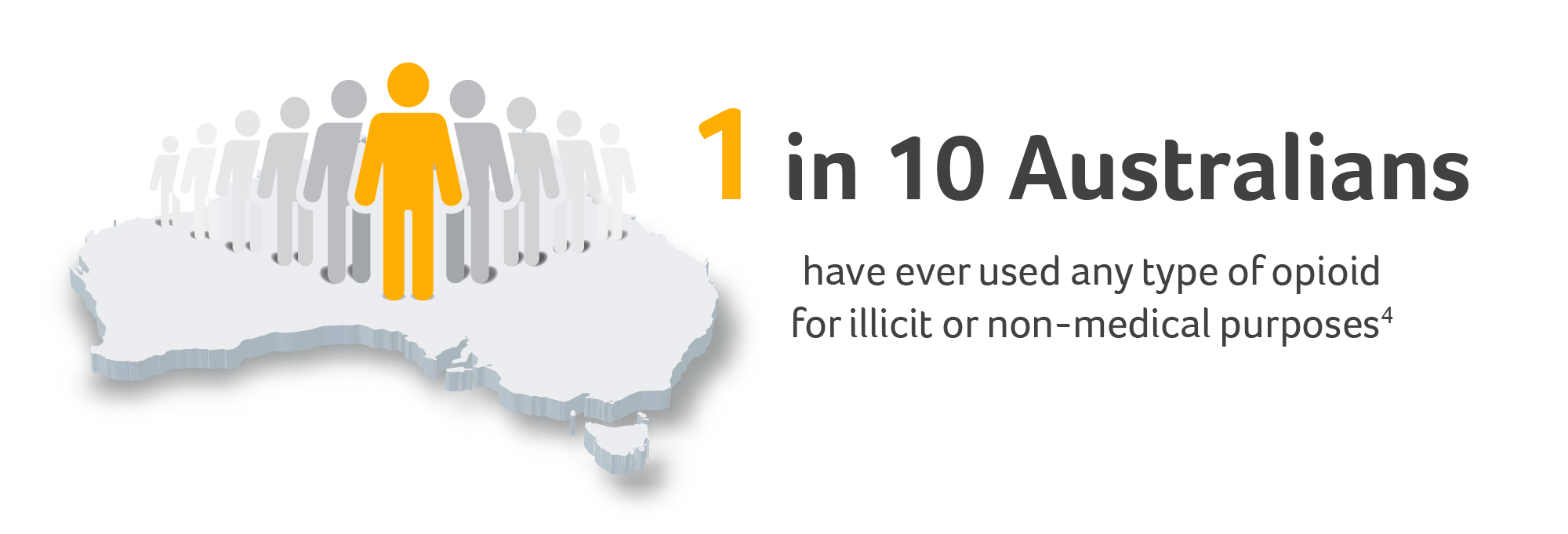
Opioid use is at an all-time high1 with 3 million people using opioids across Australia and 1.9 million estimated to initiate opioids every year2 – 50,000 of whom will cross the line from initiating opioids into persistent users in a single year.2,3*
These are extraordinary figures and set to become even more so as the annual number of opioid prescriptions continues to increase (as of 2019).1 In fact, Australia currently holds the title of the 8th highest opioid consumption internationally based on the number of defined daily doses of prescription opioids per million population.4 With that in mind, it’s hardly a surprise that as a healthcare practitioner you have likely had contact with an opioid-dependent patient – whether you realise it or not.5
All opioids – from codeine to heroin – can lead to dependence, and the consequences of leaving such dependence unchecked are dire. In Australia, people with opioid-use disorder have a crude all-cause mortality rate of 9.43/1000 patient-years and an overdose-specific mortality rate of 3.72/1000 patient-years.6 In a cohort study of people who had at least one prescription of an opioid agonist in NSW, the standardised mortality rate was alarmingly shown to be 6.06-fold higher than that observed in the general population of NSW.7 From a healthcare perspective, the Australian system sees nearly 150 hospitalisations, 14 emergency-department admissions and three deaths involving opioid harm on a daily basis.4 This amounts to a tremendous and increasing burden on the healthcare system as a whole with hospitalisations for opioid poisoning increasing by 25% over the last 10 years (2007–2008 vs 2016–2017), primarily driven by pharmaceutical-opioid hospitalisations, and the number of opioid deaths nearly doubling.4
The daily burden of opioid-use disorder4
Although 3 deaths a day might not sound like much compared with diseases like cancer (135 deaths/day) or coronary heart disease (48 deaths/day),4,8,9 it translates to 882 unintentional and, frankly, unnecessary deaths a year.10 If you think these deaths are primarily associated with illegal opium or heroin use, you would be wrong – pharmaceutical opioids account for around 50% of those deaths, an astounding 429 people a year. Although the majority of deaths were in people aged 30–49 years, almost one in three unintentional drug-induced deaths involving pharmaceutical opioids were observed in people aged 50 and above, showing that addiction transcends the ages.10
What’s more, opioid-use disorder rarely presents as a standalone disease, with two thirds of people also suffering from a mental illness. Considering that such psychiatric comorbidities further increase morbidity and mortality as well as the risk of opioid misuse and overdose, these numbers are not inconsequential.11 That’s why it is so important that opioid-use disorder is managed through an integrated model of care allowing the mental-health and substance-use issues to be addressed simultaneously. Psychosocial treatments are an essential component of all substance-use-disorder treatment programs and have a goal of helping people control the urge to use drugs and remain abstinent whilst also helping them cope with the emotional issues associated with addiction.12 Given the significant implications of opioid-use disorder on both individual well-being and the healthcare system, the implementation of effective management strategies including psychosocial treatments is essential.13
If you would like to learn more about the risks of opioid dependence, visit the TurntoHelp website for healthcare professionals.
*Based on group-based trajectory modelling.
References:
1. Therapeutic Goods Administration. Addressing prescription opioid use and misuse in Australia. 2019. Available at www.tga.gov.au/publication/addressing-prescription-opioid-use-and-misuse-australia (accessed 23 February 2022).
2. Lalic S et al. Br J Clin Pharmacol. 2019;85:202–215.
3. Lalic S et al. Br J Clin Pharmacol. 2018;84:1267–1278.
4. Australian Institute of Health and Welfare 2018. Opioid harm in Australia and comparisons between Australia and Canada. Cat. no. HSE 210. Canberra: AIHW.
5. McDonough M. Aust Prescr. 2013;36:83–87.
6. Bahji A et al. J Addict Med. 2020;14(4):e118–e132.
7. Lewer D et al. J Psychiatr Res. 2020;130:435–440.
8. Australian Institute of Health and Welfare. Cancer in Australia 2021. Available at www.aihw.gov.au/reports/cancer/cancer-in-australia-2021/summary (accessed 23 February 2022).
9. Australian Institute of Health and Welfare. Coronary heart disease. 2020. Available at www.aihw.gov.au/reports/australias-health/coronary-heart-disease (accessed 23 February 2022).
10. Penington Institute (2021). Australia’s Annual Overdose Report 2021. Melbourne: Penington Institute.
11. Jones CM and McCance-Katz EF. Drug Alcohol Depend. 2019;197:78–82.
12. Dugosh K et al. J Addict Med. 2016;10(2):93–103.
13. Rice D et al. PLoS One. 2020;15(12):e0244401.



