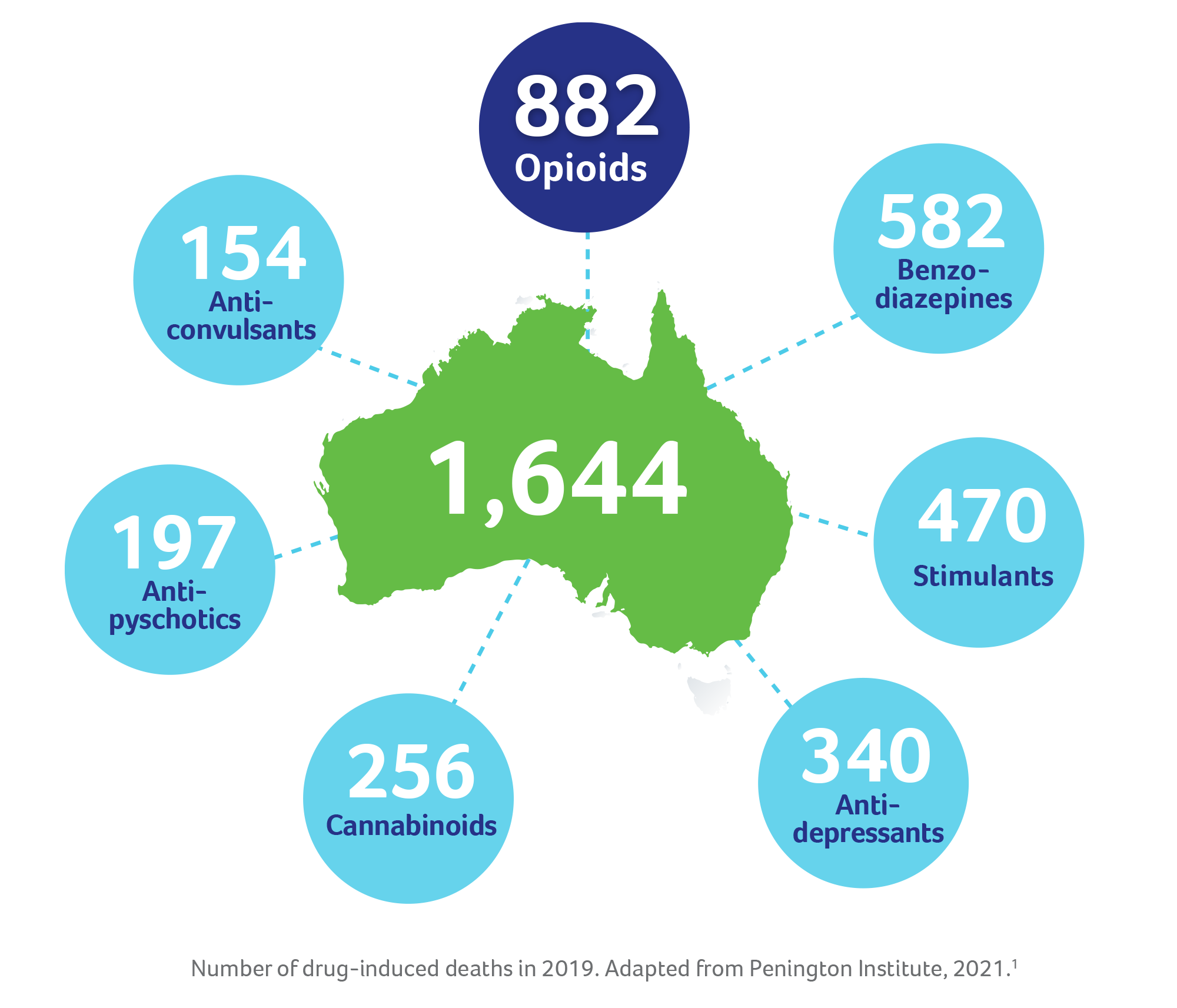
In the last decade, drug overdoses have killed more Australians than road-traffic accidents. In fact, in 2019, opioids were involved in over half of all accidental drug-induced deaths, making them the most-common cause of such deaths.1 Identifying and diagnosing opioid dependence can help connect people with the treatment they need and prevent harmful consequences, including overdose and death.2
Most healthcare professionals have likely had or will have contact with patients who have opioid dependence.3 However, not all patients will reach out for help due to fear of stigma and discrimination, and/or concerns about the legal, child-welfare, immigration, employment and/or housing ramifications.4 With this in mind, initiating patient conversation and establishing a diagnosis of opioid dependence is an important step to help patients access the help they need.
So, how can we confirm the diagnosis for opioid dependence? One way is to use the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5).5
What is the DSM-5?
The DSM-5 is a practical, functional and flexible diagnostic-tool for clinicians, covering an extensive range of mental disorders, including opioid dependence (aka opioid-use disorder).5,6 In fact, Australian and New Zealand national guidelines recognise the DSM-5 criteria as an established guide to diagnose opioid dependence.7,8
How to use the DSM-5?
In the DSM-5, opioid dependence is described as a problematic pattern of opioid use leading to problems or distress, with at least 2 of the below 11 criteria occurring within a 12-month period.5,6 11 criteria can seem like a lot to remember, so one handy mnemonic is ‘CHEW THAT COP’:5,9,10

Whilst establishing a diagnosis is important to initiate patients onto opioid-substitution therapy (e.g., methadone and buprenorphine), opioid dependence is not a standalone disease and is usually accompanied by psychological and social issues. This is why it is crucial that patients are assessed for other co-existing psychosocial conditions. The combination of medications and psychosocial support will not only treat the physical symptoms of opioid dependence, it will also provide patients a holistic treatment framework of whole-patient care.7,8
If you would like to learn more about diagnosing and recognising the signs of opioid dependence, check out the TurntoHelp website for healthcare professionals.
References:
1. Penington Institute (2021). Australia’s annual overdose report 2021. Melbourne: Penington Institute.
2. Tiet QQ, et al. Drug Alcohol Depend. 2019;198:176–179.
3. McDonough M. Aust Prescr. 2012;36:83–87.
4. Neale J, et al. Health Soc Care Community. 2008;16(2):147–154.
5. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th edn. Arlington, VA: American Psychiatric Publishing, 2013. Available at: https://www.psychiatry.org/psychiatrists/practice/dsm (accessed 22 February 2022).
6. American Psychiatric Association. Opioid use disorder. 2018. Available at: https://www.psychiatry.org/patients-families/addiction/opioid-use-disorder (accessed 22 February 2022).
7. Gowing L, et al. National guidelines for medication-assisted treatment of opioid dependence. Australian Government National Drug Strategy. 2014.
8. New Zealand practice guidelines for opioid substitution treatment. 2014.
9. National Center on Addiction and Substance Abuse at Columbia University (CASA Columbia). Overview of addiction medicine for primary care [PowerPoint presentation]. 2014. Available at: https://www.slideshare.net/centeronaddiction/overview-ofaddictionmedicineforprimarycare (accessed 24 February 2022).
10. Kadiyala PK. Gen Psychiatr. 2020;33(3):e100109.