by Dr Phoebe Holdenson-Kimura, Black Dog Institute
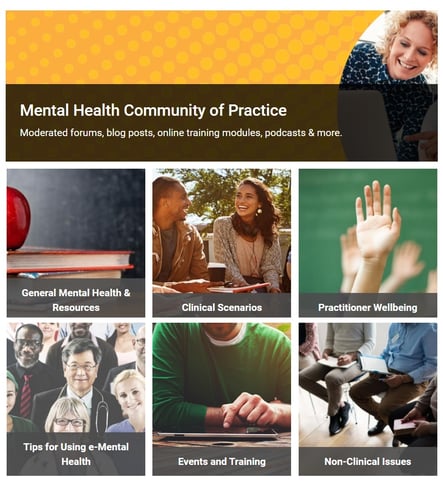
Did you know that through eMHPrac, Black Dog Institute offers an online Community of Practice, a free, welcoming online space for over 4,000 health practitioners to network, share information, support and learn from their fellow health professional community.
I quickly learned about the community when I was asked to become a moderator as part of the Black Dog Institute’s e-Mental Health in Practice program (eMHPrac). I now host webinars on e-mental health (eMH) to over 300 health professionals every month. eMHPrac is part of Australia’s response to a stepped care model of mental health treatment, where the needs of each patient are matched with the intensity of care they receive. GPs and allied health professionals are at the heart of this approach.
I first started using digital tools in practice when I was training to become a GP in rural far north Queensland. With long wait times to see the mental health professionals and a long drive to Cairns, I started offering online resources out of necessity. I quickly realised that many of my patients made positive progress more quickly than anticipated, due to the psychoeducation and cognitive behavioural therapy (CBT) skills, they were gaining from the online resources. It was quite remarkable.
Since then, I’ve worked in primary care in Cambodia and have been involved in the World Organisation of Family Doctors’ (WONCA) working party for mental health. I’ve continued to widen and promote the use of eMH tools, particularly in settings with poor mental health resourcing (sadly this is the majority of the world’s healthcare settings). However, on return to working as a GP in Sydney, I’ve realised that eMH tools are valuable in all settings – not as a replacement for face-to-face care but to supplement and equip care patients receive from their GP, psychologist or other allied health practitioner.
eMHPrac offers online training modules, webinars and e-resources designed to introduce health professionals to online programs and digital tools AND demonstrates how eMH can be integrated into primary care. I was never explicitly taught how to do this in university or vocational training, but I’m now one of those GPs that does it. It’s great to have another option in the toolkit as a GP, and I find it’s a simple, cost-effective solution for patients with mild to moderate mental health needs, I now feel confident prescribing about mental health apps and websites that can offer support, education and therapy.
The program offers a Community of Practice where we connect over 4,000 health professionals daily to offer free online resources and training as well as sharing ideas, clinical scenarios, research and peer-to-peer support.
Another great offering is the program’s free accredited Stepped Care and e-Mental Health courses. With limited access to psychologists due to geography or increased appointment wait times of up to 6 months, eMH treatments are an appropriate evidence-based option for patients with mild to moderate symptoms.
The workshops explore the resources and how to apply them in practice. Contact us at emhprac@blackdog.org.au to book in for your free, RACGP accredited courses.
The program also offers free RACGP accredited webinars, featuring national and global experts. Our upcoming webinars include:
8th December 2021 – Internet gaming disorder: Dr Vasileios Stavropoulos and Dr Hilarie Cash, register here
Sign up to our Community of Practice to receive alerts on our upcoming webinars in 2022:
- 22nd February 2022 – Digital safety planning for suicide prevention: Dr Grant Blashki and Dr Glenn Melvin
- 12th April 2022 – Integrating e-mental health tools into practice: Dr Michael Millard and Dr Jill Newby
Register now for our webinars, modules or workshops and start connecting to a community of over 4,000 health professionals.
About the Author
 Dr Phoebe Holdenson-Kimura is a GP working in Sydney who is passionate about promoting mental wellbeing and supporting GPs who have a special interest in Mental Health.
Dr Phoebe Holdenson-Kimura is a GP working in Sydney who is passionate about promoting mental wellbeing and supporting GPs who have a special interest in Mental Health.
With recent experience working in rural Far North Queensland and Cambodia, she is interested in rural and global perspectives on mental health.